Abstract
Background: Childhood obesity has become a vast concern among public health professionals. The Centers for Disease Control and Prevention reported that childhood obesity has a lasting effect on a child’s health and well-being. Research has found that 40% of Mississippi youth are obese and have a possibility of carrying the obesity into adulthood. Availability of health insurance greatly impact human health. Researchers suggest that children benefit from public and private insurance. The purpose of this study was to investigate an association between health insurance and obesity among adolescents in Hinds County, Mississippi.
Method: A cross-sectional study was administered to 36 parents of adolescents in Hinds County at the Metrocenter Mall and the Boys and Girls Club to determine whether adolescents have health insurance coverage. A descriptive statistic was conducted to describe the characteristics of the sample. Gender differences of BMI were examined using a t-test. Chi-square was used to show an association between obesity status and healthcare utilization. The statistical software that was used to analyze the data was Statistical Package for the Social Sciences (SPSS).
Results: There was no significant difference in insurance utilization and obesity rate was (p=0.125). 100% of participants with private insurance utilized their insurance while only 87% of participants utilized public insurance (p=0.056).
Conclusion: Based on this research, findings indicate that the majority of the adolescents have both public and private insurance. Parents are utilizing health insurance services for their adolescents. The prevalence of childhood obesity was significantly small. Healthcare utilization among obese adolescents was relatively small.
Keywords
License
This is an open access article distributed under the Creative Commons Attribution License which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Article Type: Research Article
EUR J ENV PUBLIC HLT, Volume 3, Issue 2, 2019, Article No: em0031
https://doi.org/10.29333/ejeph/5929
Publication date: 07 Sep 2019
Article Views: 4366
Article Downloads: 2975
Open Access HTML Content References How to cite this articleHTML Content
INTRODUCTION
Childhood obesity has become a major concern among public health professionals. The Centers for Disease Control and Prevention (2019) has reported that childhood obesity has a perpetual outcome on a child’s physical condition. The percentage of youth ages 2-19 years in the United States that are obese is estimated at 18.5% which results in 13.7 million youth (CDC, 2019). The prevalence of obesity exists in Hispanic youth at 25.8%, African American youth at 22% and Caucasian youth at 14.1% (CDC, 2019). Consequently, the higher percentage of obesity is among Hispanics and African Americans (Ogden, Carroll, Kit and Flegal, 2012). In addition, 3,600 children with obesity in the United States have developed type 2 diabetes and other communicable diseases and these problems often progress later in life (Findholt, Davis and Michael, 2013; Openchowski, 2012).
Research has found that 40% of Mississippi youth are obese and have a possibility of carrying the obesity into adulthood (Mississippi State Department of Health, 2018). Health insurance is a major contributor to healthcare access (Staiano et al., 2016). The total uninsured population in Mississippi is about 14% and it is estimated that 5% of children/adolescents fall through the gap of receiving health insurance (County Health Rankings & Roadmap, 2019). Children’s Defense Fund (2019) reported that 528,044 of qualified youth in the state of Mississippi take part in either Medicaid or Children’s Health Insurance Program (CHIP). Mississippi youth that are obese experience poor quality of life, and unhealthy behaviors (Mississippi State Department of Health, 2018).
Studies also noted that the existing cases of childhood obesity have increased among different cultures; however, it is most prevalent in minority communities (Sekhar, 2010). Proactive measures of combating childhood obesity can start with healthy behaviors. A few of these healthy behaviors include healthy eating habits, physical activity, getting enough hours of sleep, support from parents, and parents changing their lifestyle.
Parents not seeking the adequate care for their children are also of concern. Findholt et al. (2013) recognize that parents usually do not want to change their own behaviors; thereby, showing no parental involvement in the child’s health. Parents who did not have health insurance might not obtain medical care for their children with obesity because of their lack of ability to pay for the care. However, it is believed that having health insurance coverage will have a positive result on adolescents who are obese. Adolescents with obesity are usually from families who are not active on a regular basis and have poor eating habits. Promoting physical activities and good nutritional habits will benefit obese adolescents and encourage their parents to become educated surrounding childhood obesity. The researchers acknowledged that physicians can help to decrease obesity in children. Childhood obesity is an important issue in public health because public health professionals are striving to reduce obesity by providing programs that will enable children to improve their eating habits, promote education awareness, and support physical activities. Through education and the use of health insurance, primary care physicians or providers will be able to provide the counseling, nutritional planning and physical activity advice needed to fight obesity in children. Health insurance is important in providing the care needed for adolescents and family members. (Findholt et al., 2013).
Researchers have noted that children benefit from public insurance, such as Medicaid and the State Children’s Health Insurance Program (Haboush-Deloyce et al., 2014) and private insurance, such as Blue Cross Blue Shields and United Healthcare. Haboush-Deloyce et al. (2014) explained that children who attain public insurance sometimes have a difficult time accessing the care needed. According to a study recognized by the National Conference of State Legislatures (2013), obesity among children is not frequently covered by health insurance; however, having non-governmental insurance covers children and a few states take part in caring for obese children through healthcare coverage. Children qualified for Medicaid should have services provided for obesity treatment based on the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program (Lee et al., 2010). Subsequently, reducing obesity can have a positive impact on a child’s quality of life.
Limited studies have shown an impact on the utilization of health insurance among adolescents. Haboush-Deloye et al. (2014) concluded that children ages 0-5 that did not have insurance and those with public insurance had a different knowledge of their accessibility to healthcare coverage and utilization than those with private insurance. Researchers have also recognized different states where Medicaid programs treat adults with obesity; although, a few states utilize the EPSDT program which covers children with obesity (Lee et al., 2010).
Therefore, the goal of this research is to examine healthcare utilization in the context of healthcare insurance and childhood obesity among adolescents. Having access to healthcare insurance will have an impact on childhood obesity, it is important to gain this understanding because it will expand the parent’s knowledge in altering their adolescent’s lifestyle. The objectives of this study are: (1) identify types of health insurance among participants and determine the association between obesity and healthcare utilization; and (2) identify whether an adolescent has seen a physician in the past twelve months and the type of physician visits adolescents had – wellness visit, routine checkup or specific care.
METHODS
Data Collection Sampling
A non-probabilistic cross-sectional observational study was conducted to determine the association between healthcare utilization in the context of healthcare insurance and obesity among adolescents. Although it is not possible to generate unbiased estimate from the non-probabilistic sampling, it is less expensive and quick in completing the survey. Therefore, it may be reasonable to use the proposed study design for this exploratory pilot study. Data collection was performed in the Boys and Girls Club and at the Metro Center Mall both located in Hinds County, MS. A total of 61 adolescent data were obtained from 36 parents (19 in Boys and Girls Club and 17 in Metrocenter Mall) participated in the structured survey interview. Parents were informed of the purpose of the study and given a consent form to determine their willingness to participate in the study. After explaining to the parents, the reason for the study, parents had a choice to participate or not. There were no incentives given for participation. The subject selection criteria were: (a) parents living in Metro Jackson area; (b) parents who have at least one adolescent; (c) parents who are mentally stable; and (d) parents who can hear and understand questions for survey. A trained interviewer conducted face-to-face interviews to collect the data by survey. The majority of the study subjects were African American (95%), female (79%) and age of 35-44 years (54%). No site difference was observed in major demographic factors. This pilot study was approved by the Jackson State University Institutional Review Board (IRB).
Measures
Healthcare utilization was obtained by asking if the adolescent had seen a healthcare physician in the last twelve months, and whether the visit was a well care visit or a specific medical visit and if the adolescent is above his/her recommended weight for their height.
Health insurance-related information included health insurance status, medical care, type of insurance carrier, subsidies (if received), utilization of insurance carrier services, and type of services.
The body mass index (BMI) for adolescents was calculated based on an adolescent’s age or gender specifics (CDC, 2018). Therefore, the BMI of adolescents are calculated differently from adults (CDC, 2018). Based on the criteria used by CDC, each adolescent was classified as obese if their BMI was at the 95th percentile for their age and gender (CDC, 2018).
Covariates. The study survey ascertained the following information from the parents, the study participants: adolescent’s age, grade, race, height, and weight, description of health and weight condition. Parents were asked to provide their relationship status of the adolescent, gender, ethnicity, age, level of education, income status, and whether or not the adolescent lived with parent.
Statistical Analysis
Baseline characteristics of the study sample were summarized using the descriptive statistics. Mean and standard deviation for continuous variables and percentage for categorical variables were presented. Comparative analysis of key measures by demographic group was conducted using t-test for continuous variables. Gender differences of BMI were examined using an independent t-test.
We evaluated an association between healthcare utilization and obesity status using bivariate (referred to as unadjusted) and multivariate (adjusted) statistical techniques. Differences of healthcare and obesity were evaluated with χ2 tests. Because of limited sample size, we did not conduct multiple logistic regression including all potential covariates. Instead, we investigated the effect of single select covariate on the association once the significant bivariate association was found. Bar charts were presented for the graphical examination of association. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS).
RESULTS
A descriptive statistic of the characteristics of the study sample among parents and their adolescents are shown in Table 1. The study sample consists of gender, age, race/ethnicity, BMI range, income, and education level of the parents and/or adolescent. There were 21% of male parents and 79% of female parents that participated in the study. Parents reported on 51% of males and 46% of female adolescents. The percentage of adolescent’s ages 10 to 12 years old were 31%, whereas 69% were 13 to 19 years old. The majority of the participants (97%) were African American parents and adolescents and only 3% were Native Americans. Among the adolescents BMI range, 7% were underweight, 38% healthy, 25% overweight, however, 10% were obese and 21% did not report either way. Income was evenly distributed showing 25% that had an income less than $15,000, 21% whose income was up to $30,000, 26% whose income was up to $50,000 and those participants whose income was above $50,000 was reported at 24%. Parents reported the following education levels: 5% completed some high school, 15% were high school graduates, 10% has some type of trade/vocational training, 34% received an associate degree, 25% obtained a bachelor’s degree and 12% attained a master’s degree.
|
Table 1. Characteristics of the Study Sample ~ Parents and Their Adolescents
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The distribution of health indicators was completed to obtain an understanding of the frequency of the population as shown in Table 2. As parents described their adolescent’s health, the parents noted that 64% of adolescents were in great/excellent health, 31% were in good health, and 5% had fair health while no adolescent had poor health. Describing the adolescent’s weight, parents reported that 5% of adolescents were less than normal, 79% were normal, 8% were slightly heavy and 8% were overweight. Parents reported that 84% of adolescents had seen a primary care physician for wellness check-up, 7% had dental care and 2% had vision care. It was reported that 92% of the parent’s family members had health insurance and 100% of parents and adolescents had health insurance. However, 3% of adolescents received Supplemental Nutritional Assistance Program (SNAP) and Electronic Benefit Transfer subsidies. About 95% of adolescents utilize their insurance carrier services and have seen a primary care physician in the last 12 months. The percentage of primary care physicians that have spoken to adolescents about healthy eating was 77%. Parents reported that the recommended fruits and vegetables consumed daily was 84% and daily physical activity was reported at 86%. There were different types of physical activities reported such as sport activity (66%), band (8%), dance/ballet (13%), running (3%), walking (3%), and jump rope (2%).
|
Table 2. Distribution of Health Indicators
|
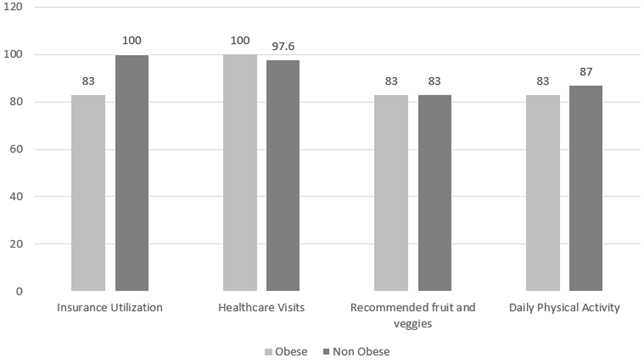
The association between obesity status and healthcare utilization was presented in Figure 1. There was no significant difference in insurance utilization and obesity rate (p=0.125); healthcare visits to primary care physicians (p>0.05); and primary care physicians speaking about healthy eating as well as adolescents consuming the recommended fruits and vegetables daily, and daily physical activity (p>0.05).
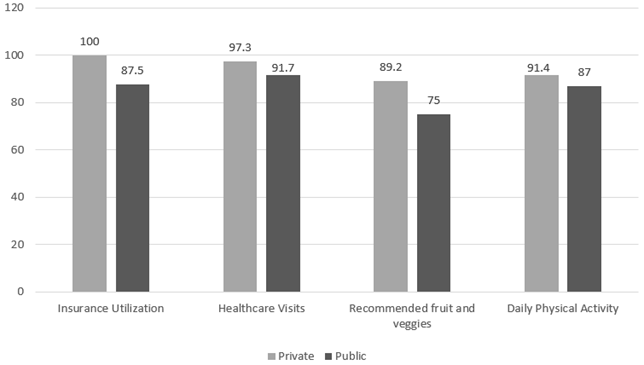
A comparison between public and private insurance and health indicators are shown in Figure 2. 100% of participants with private insurance utilized their insurance while only 87% of participants utilized public insurance (p=0.056). There was no significant difference between participants with private insurance or public insurance (p=0.556); family members with health insurance (p=0.286); and those with the recommended fruits and vegetables consumed daily (p=0.171). Furthermore, gender differences of the body mass index were also examined. There was no statistically significance between females and males in body mass index (p=0.847).
DISCUSSION
Based on this research, findings indicate that the majority of the adolescents in this study have both public and private insurance. According to Haboush-Deloye et al. (2014), the Affordable Care Act (ACA) will make healthcare available to more children. The catalyst for this new legislation centers around providing more people access to healthcare, reducing the cost of healthcare, and extending the accessibility of healthcare insurance. With the influx of newly insured Mississippians, there are opportunities for parents to utilize health insurance services for their adolescents. Therefore, this research contributes to the existing body of knowledge because it demonstrates that parents are utilizing health insurance services for their adolescents.
Adolescents in this study are involved in more healthy living and physical activity. Parents are utilizing their services by taking their adolescents to visit primary care providers. Primary care providers are engaging adolescents in discussions on healthy eating. Additionally, evidence showed that parental involvement in the child’s health has been lacking; however, in this study parent’s involvement was comprehensive. There were more adolescents with private insurance than public insurance. According to the Kaiser Family Foundation (2011), most adolescents 10-18 are covered by private insurance; this number increases significantly for adolescents with two parent households and higher income. It appeared that adolescents with private insurance utilized their insurance more than those adolescents with public insurance. Adolescents that had private insurance visited a primary care provider more than those adolescents with public insurance. Adolescent’s family members have more private insurance than public insurance. Furthermore, adolescents with private insurance are more likely to consume the recommended fruits and vegetables than those with public insurance. It appears that private insurers are utilizing insurance more readily than public insurers. Lee et al. (2010) recognize that individuals enrolled in public insurance have a higher prevalence of obesity. The prevalence of childhood obesity in this study was significantly small. Healthcare utilization among obese adolescents was relatively small. Approximately 14% of family members that were obese had health insurance.
Researchers have implied that individuals that are enrolled in Medicaid have the greatest ‘prevalence of obesity’ than individuals who do not have insurance or have private insurance (Lee et al., 2010). There are about ten states that participate in compensating for childhood obesity related health treatments; Mississippi is not among the states in the group (Lee et al., 2010). By educating the public, specifically individuals in the state of Mississippi, on preventive measures regarding childhood obesity, this may assist adolescents and parents to improve their health status.
LIMITATIONS
Limitations existed as a result of this study. It was difficult to make casual inferences in this cross-sectional study. The data was derived from self-reported information by the parents; thereby, presenting some unknown information. Stroebele et al. (2013) reported that surveys that are self-reported can be bias and are limited. Another limitation is that the accuracy of the adolescent’s weight and height was not obtained. This information was reported by the parents. Because this was a pilot study, a small number of participants were surveyed. This limited the study because it was conducted in one area in the state of Mississippi and no other areas which might have given a more diverse population. This was a convenience sampling study. Future initiatives should focus on increasing parent’s awareness and understanding of obesity healthcare services available through their insurance in rural areas verses urban areas.
CONCLUSION
Health insurance utilization effect on the prevalence of adolescent obesity in this study was significantly small. However, as a result of this study, private and public insurers had a significant impact on the utilization of health insurance and other factors that benefited the adolescent. Parents are focusing their attention on improving the adolescent’s quality of life by utilizing the insurance and services for the adolescent. Research suggests that preventative strategies will set precedence for eliminating childhood co-morbidities as well as long term health issues in adulthood (Lee et al., 2010). The opportunity to improve the quality of life for adolescents in Mississippi is important especially its community. Hence, encouraging parents to continue to utilize the services and resources available through their existing insurance will give adolescents access to strategies to improve their health.
References
- Centers for Disease Control and Prevention. (2018). About child and teen BMI. Available at: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (Accessed on July 30, 2019)
- Centers for Disease Control and Prevention. (2019). Childhood obesity facts. Available at: https://www.cdc.gov/healthyschools/obesity/facts.htm (Accessed on July 30, 2019)
- Centers for Disease Control and Prevention. (2019). Childhood obesity facts: Prevalence of childhood obesity in the United States. Available at https://www.cdc.gov/obesity/data/childhood.html (Accessed on July 30, 2019)
- Children’s Defense Fund. (2015). Children in the states 2019 – Mississippi. Available at: https://www.childrensdefense.org/wp-content/uploads/2019/04/CItS-2019_Mississippi.pdf (Accessed on July 30, 2019)
- County Health Rankings & Roadmaps. (2019). Mississippi. Available at: https://www.countyhealthrankings.org/sites/default/files/state/downloads/CHR2019_MS.pdf (Accessed July 30, 2019)
- Findholt, N. E., Davis, M. M. and Michael, Y. L. (2013). Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. The Journal of Rural Health, 29, 17-24. https://doi.org/10.1111/jrh.12006
- Haboush-Deloye, A., Hensley, S., Teramoto, M., Phebus, T. and Tanata-Ashby, D. (2014). The impacts of health insurance coverage on access to healthcare in children entering kindergarten. Maternal Child Health Journal, 18, 1753-1764. https://doi.org/10.1007/s10995-013-1420-9
- Kaiser Family Foundation (2011). Adolescent health: Coverage and access to care. Women’s Issue Brief: An Update on Women’s Health Policy. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8236.pdf (Accessed on April 2, 2019).
- Lee, J. S., Sheer, J. L. O., Lopez, N. and Rosenbaum, S. (2010). Coverage of obesity treatment: A state-by-state analysis of Medicaid and state insurance laws. Public Health Reports, 125, 596-604. https://doi.org/10.1177/003335491012500415
- Mississippi State Department of Health. (2018). 2018 Mississippi Obesity Action Plan. Available at: https://msdh.ms.gov/msdhsite/_static/resources/6164.pdf (Accessed on July 30, 2019).
- National Conference of State Legislatures. (2014). Childhood obesity legislation – 2013 update of policy options. Available at: www.ncsl.org (Accessed on July 30, 2019).
- Ogden, C. L., Carroll, M. D., Kit, B. K. and Flegal, K. M. (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. Journal of American Medical Association, 307(5), 483-490. https://doi.org/10.1001/jama.2012.40
- Openchowski, E. (2012). Linking obesity and health care. Center for American Progress. Available at: http://www.americanprogress.org (Accessed on April 2, 2019).
- Sekhar, S. (2010). The significance of childhood obesity in communities of color. Center for American Progress, 1-4.
- Staiano, A. E., Morrell, M., Hsia, D. S., Hu, G. and Katzmarzyk, P. T. (2016). The burden of obesity, elevated blood pressure, and diabetes in uninsured and underinsured adolescent. Metabolic Syndrome and Related Disorders, 14(9), 437-441. https://doi.org/10.1089/met.2016.0025
- Stroebele, N., McNally, J., Plog, A., Siegfried, S. and Hill, J.O. (2013). The Association of Self-Reported Sleep, Weight Status, and Academic Performance in Fifth-Grade Students. Journal of School Health, 2(83), 77-84. https://doi.org/10.1111/josh.12001
How to cite this article
Vancouver
Barner Y, Sung JH, Akil L, Leggett SS. Association between Health Insurance and Obesity among Adolescents. EUR J ENV PUBLIC HLT. 2019;3(2):em0031. https://doi.org/10.29333/ejeph/5929
APA
Barner, Y., Sung, J. H., Akil, L., & Leggett, S. S. (2019). Association between Health Insurance and Obesity among Adolescents. European Journal of Environment and Public Health, 3(2), em0031. https://doi.org/10.29333/ejeph/5929
AMA
Barner Y, Sung JH, Akil L, Leggett SS. Association between Health Insurance and Obesity among Adolescents. EUR J ENV PUBLIC HLT. 2019;3(2), em0031. https://doi.org/10.29333/ejeph/5929
Chicago
Barner, Yalanda, Jung Hey Sung, Luma Akil, and Sophia S. Leggett. "Association between Health Insurance and Obesity among Adolescents". European Journal of Environment and Public Health 2019 3 no. 2 (2019): em0031. https://doi.org/10.29333/ejeph/5929
Harvard
Barner, Y., Sung, J. H., Akil, L., and Leggett, S. S. (2019). Association between Health Insurance and Obesity among Adolescents. European Journal of Environment and Public Health, 3(2), em0031. https://doi.org/10.29333/ejeph/5929
MLA
Barner, Yalanda et al. "Association between Health Insurance and Obesity among Adolescents". European Journal of Environment and Public Health, vol. 3, no. 2, 2019, em0031. https://doi.org/10.29333/ejeph/5929

 Full Text (PDF)
Full Text (PDF)